Our bodies are large and complex. Cells are not concerned with complexity. They are simply needy. The broad sweeping narrative of normal cardiovascular function is delivery that is prompt, proportional and predictable. The normal heart and arteries deliver, regardless of circumstances and with little notice. Simple. There are, however, a few details.
The Arteries
James M. Wilson, MD The Heart Beat Houston MDs Neurology: 713-790-1775 Cardiology: 832-336-1530 Fax: 713-790-1605 Normal Cardiovascular Function Our bodies are large and complex. Cells are not concerned with complexity. They are simply needy. The broad sweeping narrative of normal cardiovascular function is delivery that is prompt, proportional and predictable. The normal heart and arteries deliver, regardless of circumstances and with little notice. Simple. There are, however, a few details. The Arteries The average cell needs to be bathed and refreshed constantly. Cells enjoy just such a bath that moves in a gentle to and fro, sent out from arteries and collected by veins. A heartbeat lasts a very short time, only about 1/5th of a second. In that time, roughly 4 tablespoons of blood are sent out to the arteries for delivery and the pressure in the arteries rises from 70 to 105 mmHg. Were arteries and veins simple plumbing, every bit of blood in the body would be required to move in unison in the short time of a heartbeat. The strength required to accomplish this feat would be so great that a human heart would have to have the strength of a bull. Arteries stretch and rebound. They are smarter than plumbing.
In the short time of a heartbeat, blood is shoved into the largest artery (Aorta). Blood already sitting there is pushed forward. At the same time, the artery stretches out to make more room. Instead of moving all of the blood in unison, from the heart to the smallest artery, pressure builds. Afterward, while the heart is relaxed and refilling, blood continues to be jostled about by arterial walls that are like a stretched spring. Up and down the line of arteries, stretched walls vibrate their encouragement to keep blood moving. All of the work moving blood does not have to be done in the blink of a heartbeat. Because of artery's rubber-like behavior, much of it the work accomplished during the time in between.
There is an aphorism about organizations. Sergeants run the army. Nurses run the hospital and secretaries run the world. Arterioles run the circulation. (Figure 1) They are the faucets governing flow and respond to strategic direction from nerves and hormones. For example, adrenalin makes many arterioles tighten severely so that blood will be diverted to where it is most needed. However, most of the decisions about blood flow to a tissue are made locally, without direction from nerves and hormones. Arterioles are the entry, controlling flow into the large, thin walled network of capillaries. Sitting upstream from all of the cells that they supply, arterioles can somehow sense how much blood is needed. Capillaries weep much of the fluid part of blood across their cheesecloth-like walls. The part of blood that can't cross the wall stays inside the vessel and moves along to a pool of low-pressure venules, the microscopic beginnings of the veins. There, because of the lower pressure, fluid seeps back inside of the vessel. That fluid contains waste from the cells.
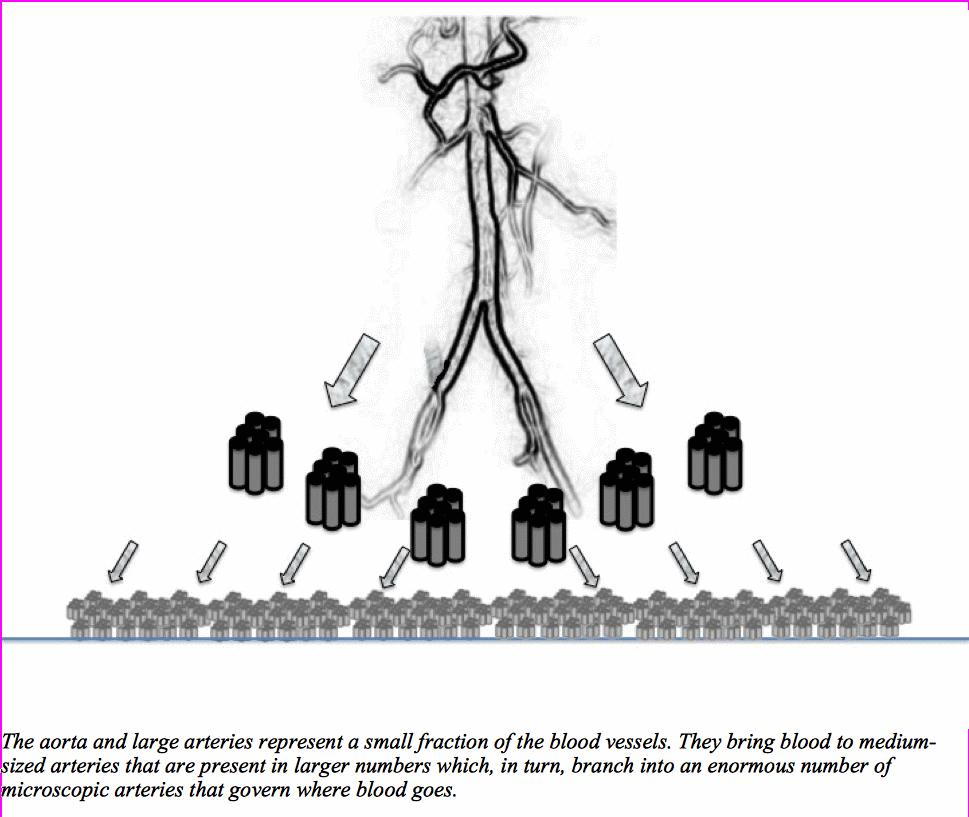
Tissue waste that includes Carbon Dioxide (CO2), adenosine and a few other things that are carried with the fluid back into blood vessels make microscopic veins relax. Relaxed veins grow larger and blood speeds away more quickly, as though running down a steeper hill. Easier out from the veins means faster flow in the capillaries and, in turn, faster flow in the arteriole. The lining of the arteriole feels the tug of the torrent and releases Nitric oxide. Nitric oxide relaxes the wall of the arteriole, opening the channel for more blood to pass. (Figure 2). This process is called autoregulation.
Large arteries absorb and distribute the blow from the heart while small arteries regulate where and how much blood may pass. Changing either of these behaviors can cause disease. More commonly, these aspects of artery function are changed in the course of a disease. For example, high blood pressure has many causes. In any individual with high blood pressure, there is rarely a single fault, but many combined. Arteries, both large and small, adapt to elevated blood pressure by increasing stiffness and thickness of their walls. The result is perpetuation of rising blood pressure regardless of its root cause(s). Meanwhile, many of the medicines that lower blood pressure act by changing either stiffness of large arteries, the opposition of small arteries or both.
The Heart
Our heart is actually two muscular pumps joined side-by-side and twisted together like a work from Escher. The two pumps are referred to as right and left for simplicity. On each side, an upper chamber (atrium) receives blood from veins and a lower chamber (ventricle) discharges it with enthusiasm into an artery. There are two sets of blood vessels connected to the heart. Both sets of vessels include both arteries and veins.
A large artery called the aorta carries blood away from the heart and on through all the needy tissues, such as the brain, muscles, intestines and kidneys. The blood collects in large veins (Vena Cava) and returns to the heart, but to the part that will send blood to the lungs. The vena cavae (there are two) is connected to the right atrium, where blood rests briefly before moving to the ventricle for discharge to the lungs. The second set of blood vessels carries blood away through the pulmonary artery, travels through the lungs and returns in pulmonary veins. Pulmonary veins are attached to the left atrium where blood rests briefly before moving to the ventricle for discharge to all points distal. Between each of the atria and their ventricles, and between each ventricle and its artery, is a valve that ensures blood will only move in one direction. Together, both sets of arteries and veins make a grand loop in a figure eight, with the heart at its center: Aorta to Vena Cava to Heart to Pulmonary Artery to Pulmonary Vein to Heart and repeat. The left ventricle is usually the principle focus of interest as the pump supplying the body. It moves blood forcefully in increments, one-quarter cup with each beat. (Figure 3)
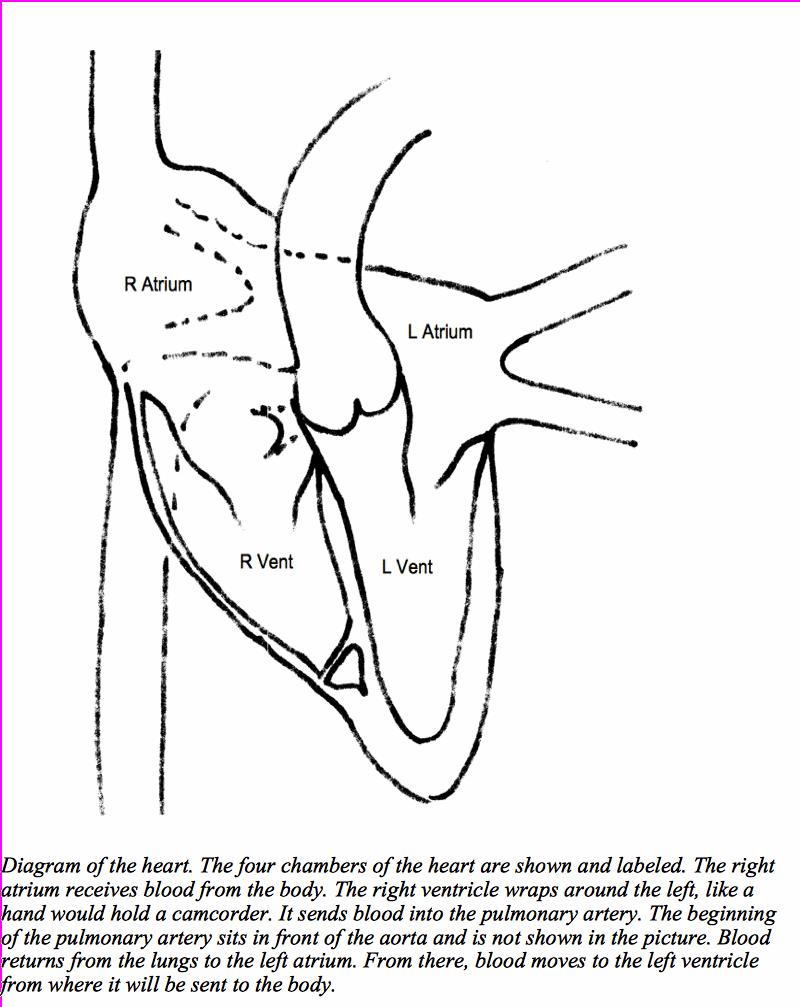
Individual heart muscle cells function simply. They shorten and relax. Laid end to end, the tiny contraction of each cell adds up to a movement of some distance. Laid side by side, their contraction has leverage that generates pressure. Archimedes claimed that, given a lever and a place to stand, he could move the world. For the heart, the shape of the pumping chamber and the thickness of the heart muscle are the lever and the place to stand. Two familiar animals offer examples of how form affects function. The frog lives life mostly prone, often in water, and minimally challenged by gravity. Its left ventricle is thin-walled and spherical, a mostly end-to-end orientation made to move large amounts of blood at low pressure. In contrast, the giraffe has a head sitting atop a long neck. This neck provides reserved seating for the finest dining, but keeps the brain at dizzying heights. In order to maintain blood flow to the brain, the heart must provide sufficient pressure to overcome the effects of gravity. As a result, its left ventricle is thick-walled with a chamber, shaped like a cylinder that is good for gripping. Although ill prepared to move large quantities, it is a very efficient pressure generator. The design of the human left ventricle lies somewhere between the cylinder and the sphere, resembling an American football.
Configuration (shape combined with muscle thickness) and the intrinsic ability of individual cells determines the heart's leverage for generating pressure and capacity to move large amounts of blood. However, each cell of the heart must follow direction. Should each tiny muscle cell act alone, the result would be a heart in wriggling chaos, without moving any blood.
Arm and leg muscles receive direction from the brain. Heart muscle cells receive direction from their neighbor. A small area of the right atrium called the sinus node awakens approximately 100 times each minute. Its awakening is a change in its electrical charge that spreads like the chime from a clock tower. As each cells feels the change, its machinery contracts even as it begins a rapid effort to return to normal. The sinus node has no other responsibility save to initiate the heartbeat.
The lights come on in the sinus node and the electrical charge moves through atrial muscle cells like a brush fire. Ventricles do the real work of sending blood out of the heart. Their contraction depends upon the spread of the same electrical charge that went through the atria. Although, the cells of the atria and ventricles lie in close proximity, they do not communicate directly. A point at the very center of the heart, where all four chambers are adjacent to one another, contains a small group of cells that bridge the communication gap. Like the sinus node, this is their only purpose. This small group of cells is the communication ?junction? between the atria and the ventricles, also known as the AtrioVentricular (AV) node. The junction was not designed for speedy communication. Its cells communicate with one another like a large group of people passing a message through a crowded room. The time required for the junction to pass along a message creates a pause between the awakening of the atria and the real work that follows in the ventricles.
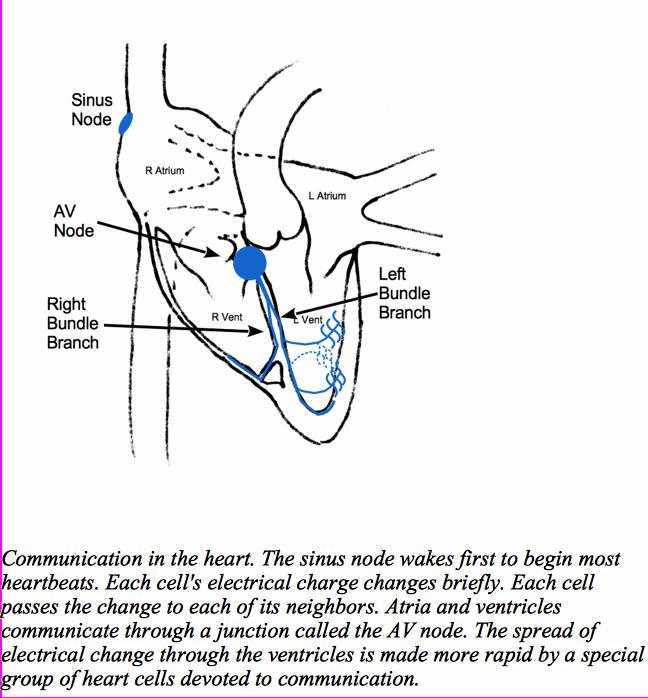
Within the ventricles there are so many muscle cells that communication, one to another, would take a very long time to make all of them move. The heart awakened in such a fashion would only suggest blood move on, rather than ejecting it. Therefore, a few muscle cells, like the cells of the sinus node and junction, have forsaken contraction and live only to pass along a message. They are arranged in long filaments. Groups of these cells, like communication cables, are called fibers. Near the junction, fibers are tightly clustered into bundles, one to the right ventricle (Right Bundle Branch) and another to the left (Left Bundle Branch). Out near the intended point of communication with working muscle, groups of these cells are called Purkinje fibers. This communication network spreads the electrical charge so quickly that all points of the ventricle move almost simultaneously. The effect is like the coordinated movement of both hands together in a clap.
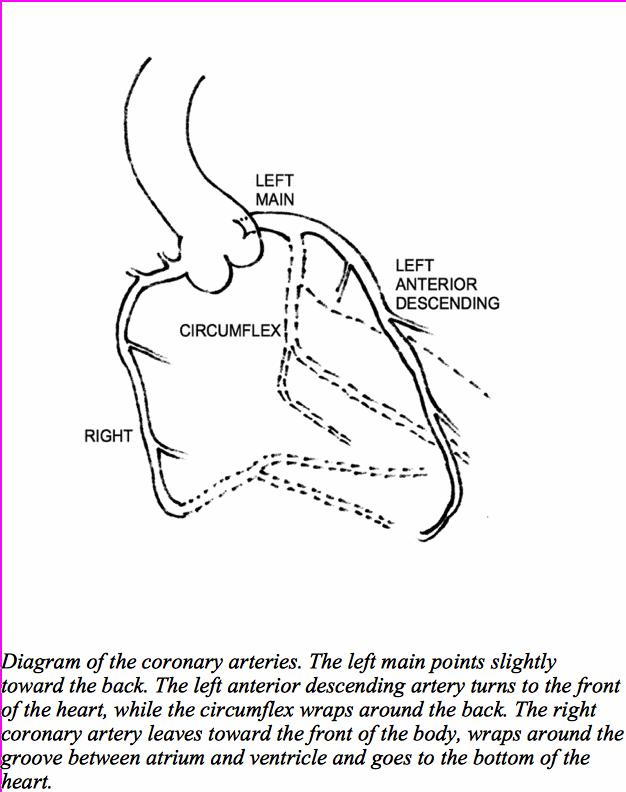
Although the human heart sees 1,800 gallons of blood going by every day, it can't drink a drop. It must be supplied by its own set of arteries. These arise from the aorta, very near its attachment to the left ventricle. From their origin, the arteries that feed the heart immediately drop down onto its surface, giving the appearance of a crown, or corona, at the base. Thus, they are known as the coronary arteries. There are two coronary arteries, one for the left side of the heart and one for the right side. They don't distribute exactly to the left and right sides and they vary from person to person, like fingerprints. (Figure 4)
Blood
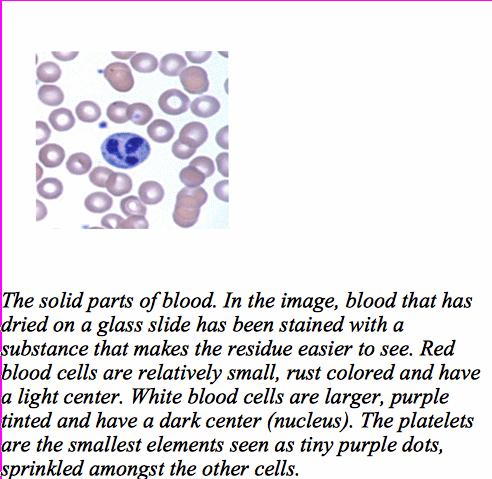
Before technology extended the capacity of observation, the workings of the body were understood through the theory of humors. Energy, animation and all the stuff of life was governed by varying mixtures of basic humors. The humors were endowed with specific powers and characteristics. They could be either hot or cold and wet or dry. Illness arose from imbalance. Their origins differed but the mixture came together in blood as the heat of life. The heat of life was understood to penetrate and enliven all tissues. Altogether, given the limits of our senses and the information available at the time, the scenario is quite reasonable. In fact, some of the conceptual imagery persists today. Something that incites waste of one's vital heat makes the blood boil. Somehow snatching that vital heat away to stop the heart makes blood run cold. There is little doubt that blood carries the stuff of life. Our understanding of that stuff is just made more sophisticated by available technology. Blood is actually a mixture of about 1/2 saltwater with dissolved substances and 1/2 suspended solids. Suspended means separates when still. In a clear tube, the sunken part is mostly dark red and the top part as a clear fluid that is golden to straw-colored. The clear, golden part, called plasma, is full of salts and proteins with a specific job to do. The parts that sink are just too large to stay water-born while sitting still for any period. Most of the sinkable part is cells or pieces of cells that are big enough to be seen under a microscope.
The most abundant cell is the red blood cell. Its job is to carry oxygen, like a boxcar on a train carries cargo. Oxygen is necessary for most basic functions, most importantly harvesting energy from food. We use almost 8 ounces of oxygen every minute, but the amount that dissolves in water is very small. Red blood cells are packed with hemoglobin, a protein that is folded around an iron atom like a catcher's mitt. In its folds, oxygen sits comfortably, making the iron just a bit more red. Red blood cells are discoid and deformable, easing their movement through the crowed spaces of small arteries and capillaries.
Fewer in number but larger in size are a group of cells with no coloring. When mixed in with the red cells, they invisible to the naked eye. All alone, their lack of coloring leaves them appearing white. These white blood cells are responsible for the body's defense. Last of the visible elements is the platelet. Where all blood cells are made, in the bone marrow, a cell devoted to sealing wholes in blood vessels grows to a great size. Pieces of it break of to enter the blood stream and perform their function. These small cell remnants are like fragments of a shattered plate, giving them their name. (Figure 4).
Protection
Nature would invade and destroy with no mercy without the constant patrol of the immune system. It is amazingly complex, precise, and effective. Immunity is pervasive. It consists of cells and dissolved proteins found in every tissue. The system was once thought to be centered on a body fluid management system called the lymphatic system. Lymph is clear fluid. Along the system's pathways are small nodules that were referred to as lymph nodes. Lymph nodes are full of cells identical to roughly half of the white blood cells found in circulation. Stained and examined under a microscope, these cells have a large, round nucleus with smooth, blue surroundings. Their resemblance to the cells populating lymph nodes gave them the name lymphocytes. Although uniform in appearance, there are a great many types of lymphocytes. They are responsible for direction, coordination and some enforcement of the immune system.
One type of lymphocyte is responsible for making antibodies. Antibodies are water loving proteins found in plasma. They are capable of recognizing virtually anything foreign to the body. Where they attach, the enforcement of the immune system is targeted, including sequestration, removal and destruction. A separate white blood cell, found in circulation, is distinguished by a sandy or granular outer appearance and a nucleus that looks like splatter (shown in Figure 4). These are destructive enforcers called granulocytes. One other type of white blood cell looks like a lymphocyte, but is much larger. In blood, it is called a monocyte. Once out among tissues, it becomes even larger and performs all enforcement functions. In tissues it is called a macrophage. Immune function participates in several heart illnesses, most notably the disease of heart valves known as Rheumatic Fever. Macrophage behavior is very important to the development and progression of atherosclerosis.
Coagulation
A coagulum is the gelatin like mass that forms from blood held in a glass tube. The blood components that create a coagulum work in circulating blood to seal fissures or fractures in blood vessels. The coagulation system works like a magic glue that moves about, sealing only when and where necessary. Some fast acting, industrial strength adhesives or glues are made of components that are so reactive with one another that they are kept physically apart until needed. When mixed, the combination is activated to its working and final state. The proteins dissolved in plasma work in a similar fashion but do not have to be physically separated before their activation. Meanwhile, once changed to their final state, they are a bell that cannot be unrung.
The components that will become biological cement mingle constantly in flowing blood. If the system were to simply be turned on and allowed to react all over, we would become a large collection of gelatin very quickly. Fortunately, the system is tightly regulated.. Coagulation proteins are washed away if they have nowhere to sit. Unprotected, they are quickly disarmed. Platelets, the small bits of cells floating about, are a special sanctuary where the glue-making coagulation proteins can get together. After platelets attach to a break in a blood vessel, they can then link together. On the surface of these platelets, the clotting system turns into glue, like masonry mortar. The mass that forms is a blood clot. In a normally functioning vessel, a clot should not form. In order to keep the clotting system from performing its task, blood is kept moving in an orderly fashion; no breaks are exposed AND the surface of a healthy blood vessel helps to disarm any wayward proteins and platelets.
Atherosclerosis, the disease responsible for heart attacks, triggers the coagulation system by exposing the underbelly of artery walls. Events like heart attack and some forms of stroke begin with platelet attachment and progress from there. Although treatment for atherosclerosis frequently employs a medicine to blunt platelet function, the fault lies in the breakdown of the artery wall, rather than with the platelets.
Energy
Energy is trapped in food, thankfully. It can?t be burned like coal to run a steam engine. So, when energy is released from food, it must be harnessed in a very particular fashion. The parts of food used for energy are carbohydrate (sugar) and lipid. Sugar is a grab bag term for substances that have a specific type of construction. They dissolve easily in water; are generally sweet to taste; may be found in different forms in many types of foods, and have names that end in ?ose, like sucrose, fructose and lactose. The sugar in milk is different from the sugar in an apple or in sugar cane. Glucose is the sugar used by the body. Burning any fuel requires oxygen. Burning the body's fuel requires oxygen to be most efficient. However, glucose can be used to release energy without oxygen. This mechanism is fast, brief and very inefficient. It is like trying to warm a room with a match.
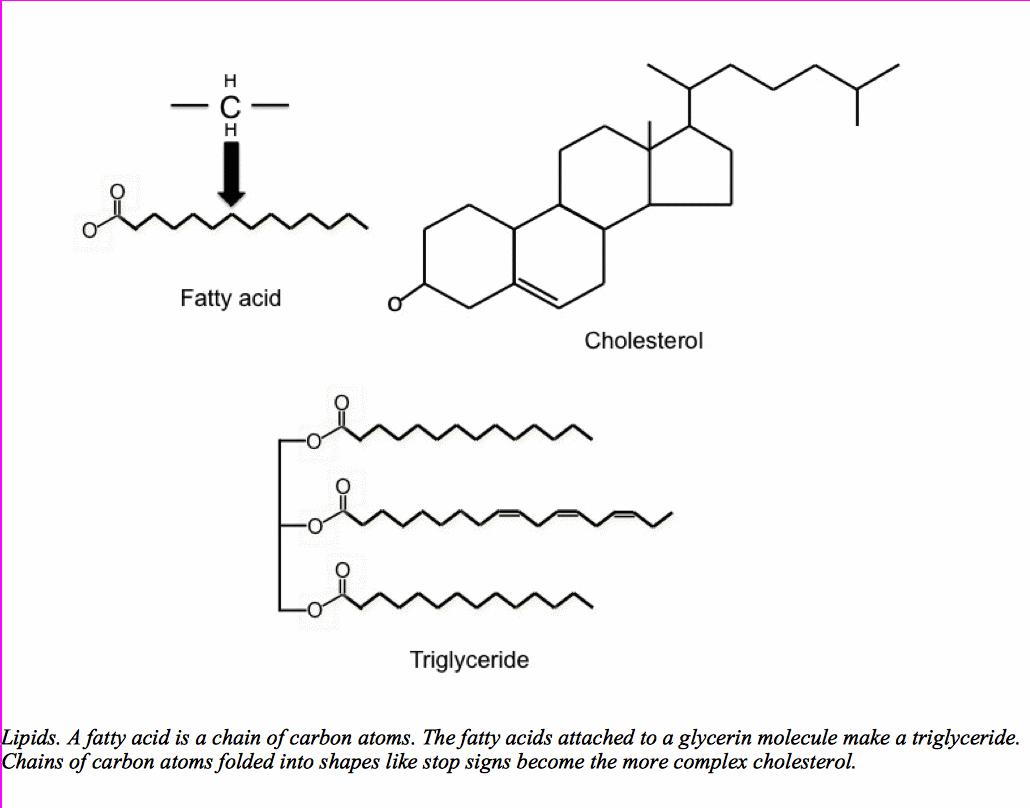
Lipid is a broad term that encompasses fats, oils, waxes and the like. However, in this discussion, any mention of lipids is in reference to fatty acids, triglyceride and cholesterol. A fatty acid is a long molecule with one end that likes to associate with water and an oily tail that is shaped like a pipe cleaner bent into a zigzag. The long oily tails are none to fond of water, but love one another. They are stored by attaching fatty acid to a sugar-like molecule called glycerin. There are only three places to add a fatty acid to glycerin. Therefore, the complex is called a Tri-glyceride. Dietary sources of fatty acid and triglyceride abound, including meat, dairy, and plant fats.
The liver coordinates energy storage and distribution. It processes triglyceride from the diet. However, it may also convert surplus glucose to fatty acid and attach surplus fatty acid to glycerin. Glucose is distributed easily because it is soluble in water. Fats float, making transportation through the watery bloodstream difficult. Therefore, the liver packages them in special capsules whose outside lining has an affinity for water. The capsules, called lipoproteins are complex. Mixed into the surface coating are a group of handles that cells use to recognize the lipoprotein and extract its contents. (Figure 6)
Cholesterol is a chain of carbon atoms folded into shapes instead of long oily tails. The shapes make cholesterol useful in the construction of hormones and cell membranes. Most of the body's cholesterol is made in the liver rather than being taken in through diet. However, like triglycerides, it interacts poorly with water and must be transported to cells in a lipoprotein capsule.
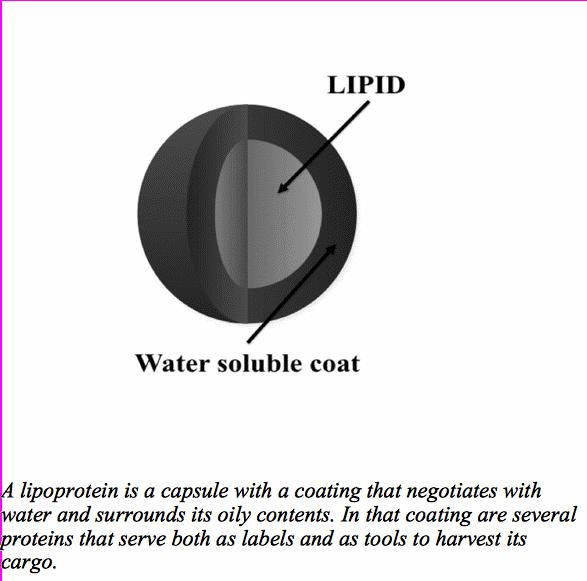
The capsules are named based upon where they land after a trip through a centrifuge. The force applied to blood placed in a centrifuge is enormous. Contents exposed to that force order themselves according to size and density, softballs at the top and golf balls at the bottom. The capsules that carry lipid out of the liver are large and fluffy. They have the very clever name, Very Low Density Lipoprotein (VLDL). After a tour of the body, VLDL gives away some of its triglyceride. It becomes the smaller, denser, Low Density Lipoproteins (LDL) that still has plenty of cholesterol. LDL continues to make deliveries and is eventually taken back by the liver. The smallest and densest capsule is called High Density Lipoprotein (HDL). HDL is sent from the liver virtually empty. Its task is to bring lipid to the liver.
Abnormal energy metabolism traps many of its components in circulating blood. Excess glucose impairs tissue function throughout the body. It may also attach itself to a variety of proteins, furthering its dysfunctional influence. Lipoproteins in excess accumulate where they do not belong. The attemps to clear them away is one of the driving forces behind the development of atherosclerosis and heart attack. This is a brief, general description of basic functions affecting and affected by the heart and arteries. Each function is important in the pursuit of basic health maintenance as well as understanding most of the common forms of heart disease.



